DALGARNO RESEARCH REPORTS
Dalgarno Institute Research Reports are a great resource that aims to provide current research to users. The reports take key up-to-date evidence-based data relating to Alcohol and Other Drug issues and deliver it in a format that is easier to use for reference purposes. The data may have some commentary, but is generally representative of source evidence, whilst culling the extraneous. All data in the reports is referenced and cited so as to enable the user to further investigate the topic/issue if required.
Check out the complete collection of Research Papers and other useful material visit Dalgarno Institute Website
Trends in alcohol, MDMA, methylamphetamine and THC in injured and deceased motor vehicle drivers and motorcyclists over a decade (2010–2019) in Victoria, Australia
Abstract:
Background Driving under the influence of alcohol and other drugs contributes significantly to road traffic crashes worldwide. This study explored trends of alcohol, methylamphetamine (MA), 3,4-methylenedioxy-N-methylamphetamine (MDMA) and Δ9-tetrahydrocannabinol (THC), in road crashes from 2010 to 2019 in Victoria, Australia.
Methods We conducted a cross-sectional analysis using data from the Victorian Institute of Forensic Medicine and Victoria Police, examining proscribed drug detections in road crashes. Time series graphs per substance explored indicative trends and comparisons between road users. Negative binomial regression models, with robust SEs and adjusted for exposure (kilometres travelled, Victorian licence holders), modelled the incidence rate ratio, with a Bonferroni-adjusted α=0.007 for multiple comparisons.
Results There were 19 843 injured drivers and 1596 fatally injured drivers. MA had the highest prevalence (12.3% of fatalities and 9.1% of injured drivers), demonstrating an increase over time. Overall, 16.8% of car drivers and motorcyclists tested positive for one or more drugs, with 14% of crashes involving a blood alcohol concentration (BAC)≥0.05%. MA and THC were the most common drugs in fatalities. Between 2015 and 2019, MA was detected in 27.9% of motorcyclist fatalities, followed by THC (18.3%) and alcohol ≥0.05% (14.2%), with similar but lower frequencies among injured motorcyclists. Alcohol detections (≥0.05% BAC) in fatalities declined, but increased in injured motorcyclists and car drivers until plateauing in 2017. THC detections rose among injured drivers until 2018, detected in 8.1% and 15.2% of injured and fatal drivers, respectively. MDMA-positive driving decreased among injured drivers and remained stable at ~1% of fatalities.
Conclusions Despite enhanced road safety measures in Victoria, drug-driving persists, indicating a need for revised prevention strategies targeting this growing issue.
(Source: BMJ JOURNALS)
PREVENTION & Demand Reduction Must Be the Prioirity of Community Drug Policy
Originating in the US, Communities that Care is a public health prevention framework that has been operating in Australia for 25 years.
Over 30 Local Government Areas have used the framework to reduce alcohol consumption, injuries and crime. In the US it has been used to also reduce smoking, cannabis and depression. An Australian cost benefit analysis has shown that using the CTC approach to adolescent alcohol consumption has a return of investment of $2.60.
This presentation outlines the Communities that Care model and how communities can use the model. It also presents findings from the National Australian Cluster Randomised Control Trial, and other national and international longitudinal evidence. (Watch Webinar Here)
Also see
- Why Prevention Matters and to Whom
- AOD Primary Prevention & Demand Reduction Priority Primer
- Asia-Pacific Prevention Hearing 2024 – The Declaration of Oviedo
- Prevention Basics! #Prevention #Childfirst What Adults Need to Know — One Choice Prevention
- Protective Factor Number One in Drug Use Prevention Science
- Prevention & Demand Reduction: Denying or Delaying Substance Use in Communities – An Evidence-Based Best Practice Guide'

HARM REDUCTION – Australia’s Drug Policy Dilemma – Time for Prevention, Demand Reduction, and Recovery
 In what might go down as the most expensive experiment in missing the point, Australia’s decades-long dance with harm reduction policies has produced results that would be laughable if they weren’t so tragic. New data reveals a sobering reality: whenever harm reduction takes centre stage, drug-related deaths perform their own tragic encore.
In what might go down as the most expensive experiment in missing the point, Australia’s decades-long dance with harm reduction policies has produced results that would be laughable if they weren’t so tragic. New data reveals a sobering reality: whenever harm reduction takes centre stage, drug-related deaths perform their own tragic encore.
Historical Context: Australia’s Drug Policy Journey
The trajectory of Australia’s drug policy reads like a cautionary tale in unintended consequences. Between 1985 and 1999, as Australia embraced harm reduction approaches, it achieved an unfortunate distinction: the highest drug use rates among OECD countries. The numbers tell a stark story – opiate deaths rose from 347 in 1988 to 1,116 in 1999, a trajectory that should have set off alarm bells throughout the public health community.
However, a brief period of hope emerged between 1998 and 2006, when Australia implemented the Federal Prevention approach. During this period, deaths from all drug types decreased significantly. This success was short-lived. From 2007 onward, with the return to harm reduction priorities, death rates began climbing again across all drug categories.
The harm reduction movement’s reliance on questionable scientific methodology deserves scrutiny. Consider the 2011 Lancet study on Vancouver’s injecting room, which claimed a 9% reduction in overdose deaths. Official British Columbia coroner’s figures tell a different story:
- 2001: 90 overdose deaths
- 2002: 49 deaths
- 2003: 51 deaths
- 2004: 67 deaths (37% increase after facility opened)
- 2005: 55 deaths (still 12% higher than pre-facility)
The study’s methodology artificially created positive results by comparing different time periods in a way that obscured the actual impact of the facility.
Current Harm Reduction Proposals: A Critical Examination
Pill Testing: The Dangerous Illusion of Safety
Proponents of pill testing present it as a scientific solution to drug-related deaths. However, a comprehensive analysis of 392 Ecstasy-related deaths in Australia between 2000 and 2018 reveals the fundamental limitations of this approach:
- 14% of deaths resulted from allergic-type reactions that no pill testing regime could predict
- Nearly half (48%) of deaths involved polysubstance use, particularly combinations with alcohol and cocaine
- 29% of deaths occurred due to accidents while intoxicated
These statistics highlight a crucial flaw in the pill testing paradigm: it creates a false sense of security while being unable to prevent the primary causes of Ecstasy-related deaths. The very presence of pill testing facilities may inadvertently legitimise drug use, suggesting to potential users that there exists a “safe” way to consume illegal substances.
Injecting Rooms: The Statistics That Don’t Add Up
Perhaps nowhere is the failure of harm reduction more evident than in the statistics surrounding injecting facilities. The Sydney injecting room reported overdose rates 63 times higher than the pre-registration rates of its clients – a number that defies logical explanation. Melbourne’s Medically Supervised Injecting Room (MSIR) reported even more troubling numbers, with overdose rates 102 times higher than street rates.
These statistics raise serious questions:
- How do these facilities actually prevent harm when they appear to be associated with increased risk-taking behaviour?
- Are these facilities inadvertently creating “safe spaces” for dangerous behaviour rather than reducing it?
- Does the presence of medical supervision encourage users to take greater risks?
The 2020 government-funded evaluation of Melbourne’s MSIR revealed another troubling trend: deaths actually increased in the facility’s area, mirroring increases across Melbourne. This suggests that rather than preventing deaths, these facilities may be prolonging dangerous drug use patterns, ultimately leading to greater loss of life.
The International Experience: Cautionary Tales
Portugal’s Decriminalisation: A Closer Look at the Data
Portugal’s 2001 drug decriminalisation policy is often cited as a model for drug policy reform. However, a detailed examination of the outcomes reveals concerning trends:
- Overall drug use has increased by 59% since implementation
- Minor drug use has seen increases of up to 80%
- Overdose deaths have risen by 85% since 2002
- Portugal now ranks among the top three EU countries for illegal drug use in wastewater testing
These statistics stand in stark contrast to the narrative of success often presented by harm reduction advocates. The Portuguese experience suggests that removing criminal penalties, while maintaining technical illegality, creates a confusing middle ground that may actually increase drug use and associated harms.
The Colorado Cannabis Experiment: Unintended Consequences
Colorado’s journey with cannabis liberalisation provides another warning about the potential consequences of harm reduction approaches. Following medical cannabis law loosening in 2009 and full legalisation in 2013, the state experienced:
- A 410% increase in cannabis-related suicides by 2016
- A 360% increase in cannabis-related hospitalisations
- A 230% increase in cannabis-related traffic deaths
- A doubling of adult cannabis use
These numbers suggest that policies intended to reduce harm may instead normalise drug use and increase overall societal costs.
Evidence-Based Success Stories: What Actually Works
While the failure of harm reduction approaches is clear, several jurisdictions have demonstrated remarkable success with prevention-focused policies:
- Sweden achieved an 80% reduction in secondary student illicit drug use between 1971 and 1990 through a consistent focus on prevention and clear anti-drug messaging.
- Iceland’s prevention-focused approach resulted in a 60-90% reduction in secondary student illicit drug use from 1998 to present.
- Australia achieved a 40% reduction in both student and adult drug use during the “Tough on Drugs” period (1998-2007).
- The US much-maligned but effective “Just Say No” campaign achieved a 70% reduction in secondary student use between 1981 and 1991, demonstrating the power of clear, consistent messaging.
Time for Change: The Path Forward
As Australia approaches another Drug Summit, policymakers face a critical choice. The evidence clearly shows that harm reduction policies, despite their compassionate intentions, have failed to deliver on their promises. Instead, they have often contributed to increased drug use, higher death rates, and greater societal costs.
The success stories from Sweden, Iceland, and Australia’s own “Tough on Drugs” era provide a clear roadmap for effective drug policy:
- Prioritise prevention over harm reduction
- Implement clear, consistent anti-drug messaging
- Maintain strong legal deterrents while providing appropriate treatment options
- Focus on reducing overall drug use rather than merely managing its consequences
The time has come to acknowledge that enabling drug use while calling it “harm reduction” has failed. The data shows that Prevention, Demand Reduction, and Recovery aren’t just buzzwords – they’re proven lifesavers. The cost of maintaining failed harm reduction policies is measured not just in dollars, but in lives lost and potential squandered. It’s time for a return to these evidence-based strategies that have demonstrated real success in reducing drug use and its associated harms. (WRD News November 6th 2024thWRD News November 6th 2024)
Also see
Psychiatric risks for worsened mental health after psychedelic use
Background: Resurgent psychedelic research has largely supported the safety and efficacy of psychedelic therapy for the treatment of various psychiatric disorders. As psychedelic use and therapy increase in prevalence, so does the importance of understanding associated risks. Cases of prolonged negative psychological responses to psychedelic therapy seem to be rare; however, studies are limited by biases and small sample sizes. The current analytical approach was motivated by the question of whether rare but significant adverse effects have been under-sampled in psychedelic research studies.
Results: We find that 16% of the cohort falls into the “negative responder” subset. Parsing the sample by self-reported history of psychiatric diagnoses, results revealed a disproportionate prevalence of negative responses among those reporting a prior personality disorder diagnosis (31%). One multivariate regression model indicated a greater than four-fold elevated risk of adverse psychological responses to psychedelics in the personality disorder subsample (b = 1.425, p < 0.05).
Conclusion: We infer that the presence of a personality disorder may represent an elevated risk for psychedelic use and hypothesize that the importance of psychological support and good therapeutic alliance may be increased in this population.
(Source: https://journals.sagepub.com/doi/epub/10.1177/02698811241232548 )
Transition to Schizophrenia Spectrum Disorder Following Emergency Department Visits Due to Substance Use With and Without Psychosis – Cannabis Tops the List
Question: What is the risk of developing schizophrenia spectrum disorder following an emergency department (ED) visit caused by substance use with and without psychosis?
Findings: In this cohort study of 9.8 million people, individuals with an ED visit for substance-induced psychosis or substance use without psychosis were at increased risk of developing schizophrenia spectrum disorder within 3 years relative to the general population.
Meaning: These findings suggest that people who present to the ED for substance use, with or without psychosis, are at increased risk of developing schizophrenia spectrum disorder.
Abstract
Importance: Episodes of substance-induced psychosis are associated with increased risk of developing a schizophrenia spectrum disorder. However, there are limited data on the transition risk for substance use without psychosis.
Objectives: To quantify the risk of transition to schizophrenia spectrum disorder following an incident emergency department (ED) visit for (1) substance-induced psychosis and (2) substance use without psychosis and to explore factors associated with transition.
Results: The study included 9 844 497 individuals, aged 14 to 65 years (mean [SD] age, 40.2 [14.7] years; 50.2% female) without a history of psychosis. There were 407 737 individuals with an incident ED visit for substance use, of which 13 784 (3.4%) ED visits were for substance-induced psychosis. Individuals with substance-induced psychosis were at a 163-fold (age- and sex-adjusted hazard ratio [aHR], 163.2; 95% CI, 156.1-170.5) increased risk of transitioning, relative to the general population (3-year risk, 18.5% vs 0.1%). Individuals with an ED visit for substance use without psychosis had a lower relative risk of transitioning (aHR, 9.8; 95% CI, 9.5-10.2; 3-year risk, 1.4%), but incurred more than 3 times the absolute number of transitions (9969 vs 3029). Cannabis use had the highest transition risk among visits with psychosis (aHR, 241.6; 95% CI, 225.5-258.9) and the third-highest risk among visits without psychosis (aHR, 14.3; 95% CI, 13.5-15.2). Younger age and male sex were associated with a higher risk of transition, and the risk of male sex was greater in younger compared with older individuals, particularly for cannabis use.
Conclusions and Relevance: The findings of this cohort study suggest that ED visits for substance use were associated with an increased risk of developing a schizophrenia spectrum disorder. Although substance-induced psychoses had a greater relative transition risk, substance use without psychosis was far more prevalent and resulted in a greater absolute number of transitions. Several factors were associated with higher transition risk, with implications for counseling and early intervention
(Source: JAMA Psychiatry | JAMA Network 2023)
The use of psychedelic drugs to treat mental illness is allowed in Australia, but confusion remains.
Months after Australia found itself at the global forefront of work to treat mental illness using psychedelic substances found in illicit drugs like ecstasy and magic mushrooms, those working in the field say confusion is rife.
A surprise decision by the country's drug regulator to approve the use of the substances, which caught even those working in the field unawares, came into effect on July 1.
Months after Australia found itself at the global forefront of work to treat mental illness using psychedelic substances found in illicit drugs like ecstasy and magic mushrooms, those working in the field say confusion is rife.
A surprise decision by the country's drug regulator to approve the use of the substances, which caught even those working in the field unawares, came into effect on July 1.
Since then, public interest in the use of MDMA and psilocybin to treat conditions like PTSD and treatment-resistant depression has grown while mental health practitioners try to navigate the unexpected change — with some flagging "serious reservations".
As issues around how treatment should be administered, who should be able to access the tightly-controlled substances and how much treatment should cost remain unclear, a body of medical and health practitioners has called for an urgent industry meeting to help iron out the problems.
Some say 'premature' decision has led to 'virtually unworkable' system
Anthony Bloch chairs the Australian Multidisciplinary Association for Psychedelic Practitioners (AMAPP), a 160-member organisation formed in the wake of the decision by the Therapeutic Goods Administration (TGA).
He said the group understood the TGA decision was "both unexpected and perhaps premature" given "the lack of adequate research up until now into psychedelic medicines".
But Dr Bloch said in light of the decision having been made, the group is calling for an urgent meeting to be held with the TGA, the Royal Australian and New Zealand College of Psychiatrists (RANZCP) and state health departments to help improve how things are working.
"The current regulatory system is virtually unworkable, overly cautious and cumbersome and needs to evolve with the help and input from those practitioners who have appropriate knowledge and experience working in the psychedelic field," he said.
The TGA said it was "always open to meet with stakeholders in order to help overcome points of confusion that may exist" and had met with stakeholders regarding the use of psilocybin and MDMA.
"The TGA welcomes an expression of interest to meet with any organisation should they wish to seek further discussion on these issues," they said.
RANZCP president Elizabeth Moore said guidance developed by the body regarding psychedelic-assisted therapy involved consultation with experts, "with patient safety as the primary concern and number one priority".
"Use of psychedelic-assisted therapy may carry its own unique risks that necessitate careful clinical judgement."
Dr Moore said the RANZCP was committed to safe practice and would meet with stakeholders as appropriate.
There is confusion about how treatment gets administered
For people who manage to access the treatment, the process is not a simple case of being handed a script.
Psychedelic-assisted treatment requires intensive preparation and supervision and trusting relationships with the mental health practitioners involved.
Experts say about 20 hours is the minimum requirement for a course of treatment.
Under the changes, only authorised prescribers — psychiatrists approved by the TGA — are able to access and administer MDMA and psilocybin.
Dr Bloch said he understood that less than 10 psychiatrists across Australia had been authorised as prescribers.
"While we understand the caution, limiting prescribers to that level of involvement in psychedelics does not add to safety, in our opinion," he said.
"All it does is completely restrict access."
He also said the level of involvement expected from the authorised prescribers was out of sync with the way mental health treatment worked on the ground.
According to the TGA, the authorised prescribers "must be directly involved in the immediate care of every patient undergoing treatment". That includes patient screening and consent, accessing the drugs for treatment and assessing the treatment.
Dr Bloch said the role supporting mental health practitioners could play in treatment was unclear, as were the settings for psychedelic-assisted therapy.
"Some state governments are now saying the clinics have to be inpatient facilities, while other state governments are saying they can just be day clinics," he said.
The research behind MDMA and psilocybin differs
Psychiatrist Nigel Strauss, who has been involved in psychedelic therapy for more than a decade, said the body of research behind the use of MDMA to treat PTSD is quite well established compared with the use of psilocybin to treat depression.
And he said the drugs worked differently.
"Psilocybin is a true psychedelic and I think there's a need for more research on who is suitable for this treatment, to discover outcomes and so forth," Dr Strauss said.
"Even though the TGA have announced that we can use it in treatment-resistant depression, I think there is some concern that there's still more to be learned about how we select people for this treatment, and how the treatment is carried out."
A Swinburne University study involving about 160 participants trialling the use of psilocybin for depression is about to begin.
Dr Strauss said such studies — the approval of which is separate to the TGA decision — were crucial to informing the use of the drug in one-on-one therapeutic settings.
"The results of that will tell us a lot about the effectiveness of the drug, but also to help to train a number of therapists," he said.
Public interest has geared up
Since the TGA's decision, public interest in psychedelic-assisted therapy (PAT) treatments has spiked.
One of the few psychiatrists authorised to prescribe the drugs, who wanted to remain anonymous, said they had a waiting list of 400 people interested in accessing the treatment.
"They won't all be eligible or ideal candidates — however, they are people who have tried every available mental health treatment and are interested in psychedelic-assisted therapy," they wrote.
Another practitioner said they received about 10 enquiries a week, with that figure jumping to about 30 "immediately after any news/Netflix special, etc".
Amid the increased interest is also a lack of understanding about the strict criteria that means many will not be eligible.
One practitioner reported that their client had told them that when they saw a psychiatrist the next month for their ADHD "they were going to ask … for a script of psilocybin so they could start microdosing".
The cost is still prohibitive for individuals
Given the intensive nature of psychedelic-assisted therapy, and the lack of subsidies in place for access to the drugs, the cost can run into thousands of dollars, making it too expensive for most people to access.
Dr Strauss said as well as the long-term goal of attracting a "meaningful" Medicare rebate, there were opportunities for other funding sources to help individuals access care as the use of the drugs becomes more established.
"Ideally, we want to see the Department of Veterans' Affairs, other first responder organisations starting to fund their members' PTSD treatments," he said
"We want to see private health insurers jumping in and realising that funding a person's treatment-resistant depression for a lifetime is more expensive than a psychedelic assisted therapy which may put them in remission for years, or longer, from a single treatment."
Further Reading
- Psychedelics: The New Panacea – Just Like Cannabis, it will Fix Everything, Won’t it?
- Psychedelics: The Hype, The Hope, The Harm? – Is the therapeutic potential of hallucinogens risky and overhyped?
- History repeating: A Roadmap to Address Common Problems in Psychedelic Science
- Problematic Psychedelics – Prescribing Harm? Researchers Warn of Major Threats to the Validity of Psychedelic Research
- We don’t want to run before we walk
“We don’t want to run before we walk”: the attitudes of Australian stakeholders towards using psychedelics for mental health conditions
Conclusions: Stakeholder representatives and politicians agree that insufficient evidence exists to support the widespread clinical implementation of psychedelics in Australia. Politicians also perceive the stigma associated with psychedelics might negatively influence progressive legislation. Additional research and a clear presentation of this research are needed before the clinical use of psychedelics can be supported. (Source: Public Health Research & Practice)
Psychedelics, much like cannabis, has been touted by activists as a new panacea for many ills. However, as with all such activism and a new 'vote for medicine' wedge into our pharmaceutical system, we are seeing less, not more thorough, double-blind, placebo accounted for clinical trials. The hyped promises and now wielded 'anecdata' of subjective testimonies are thinly draped over the growing body of evidence that these substances are not only under-delivering, but in growing numbers of cases, very damaging.
History repeating: A Roadmap to Address Common Problems in Psychedelic Science
Abstract: Research in the last decade has expressed considerable optimism about the clinical potential of psychedelics for the treatment of mental disorders. This optimism is reflected in an increase in research papers, investments by pharmaceutical companies, patents, media coverage, as well as political and legislative changes. However, psychedelic science is facing serious challenges that threaten the validity of core findings and raise doubt regarding clinical efficacy and safety. In this paper, we introduce the 10 most pressing challenges, grouped into easy, moderate, and hard problems. We show how these problems threaten internal validity (treatment effects are due to factors unrelated to the treatment), external validity (lack of generalizability), construct validity (unclear working mechanism) or statistical conclusion validity (conclusions do not follow from the data and methods). These problems tend to co-occur in psychedelic studies, limiting conclusions that can be drawn about the safety and efficacy of psychedelic therapy. We provide a roadmap for tackling these challenges and share a checklist that researchers, journalists, funders, policy makers, and other stakeholders can use to assess the quality of psychedelic science. Addressing today’s problems is necessary to find out whether the optimism regarding the therapeutic potential of psychedelics has been warranted and to avoid history repeating itself.
False Claims for Portugal and Decriminalisation
“The mantra repeated by worldwide media, which has demonstrated that truth is no longer their interest, is that Portugal’s drug decriminalisation has been an unmitigated success. But their policies of ‘dissuasion’ have clearly not reduced drug use as they wanted. Rather drug use has increased 59% since 2001 when they first decriminalised. On their own terms, this is failure.”
Also see
- 20 years of Portuguese Drug Policy – Development & Challenges
- How the former 'heroin capital of Europe' decriminalised drugs
- Portugal Drug Policy – A Review Of The Evidence: Highlights Many Problems that Make it Unsuitable for Australia
Is the Psychedelic Therapy Bubble About to Burst?
A new paper argues that excitement has veered into misinformation—and scientists should be the ones to set things straight.
CONCLUSIONS: On the basis of the change in depression scores on the QIDS-SR-16 at week 6, this trial did not show a significant difference in antidepressant effects between psilocybin and escitalopram in a selected group of patients. Secondary outcomes generally favored psilocybin over escitalopram, but the analyses of these outcomes lacked correction for multiple comparisons. Trial of Psilocybin versus Escitalopram for Depression | NEJM
IN APRIL 2021, a widely anticipated paper in the field of psychedelics dropped. The study, a small trial run at Imperial College London and published in The New England Journal of Medicine, investigated the use of psilocybin, the active ingredient in magic mushrooms, to treat depression. Led by Robin Carhart-Harris, who now directs the Neuroscape Psychedelics Division at the University of California, San Francisco, the research compared psilocybin with a standard antidepressant. The findings were somewhat lackluster: it found that the psychedelic was only marginally better than traditional treatments at relieving depression.
Back in 2017, Rosalind Watts, an author on that paper and a former clinical lead for the trial at Imperial, had given a TEDx talk on the power of psilocybin to treat depression, prompted by the time she had spent working on the study. In the talk, she shared her belief that psilocybin could “revolutionize mental health care.” But in February of this year, Watts published a Medium piece in which she expressed regret at her initial unbridled enthusiasm. “I can’t help but feel as if I unknowingly contributed to a simplistic and potentially dangerous narrative around psychedelics; a narrative I’m trying to correct,” she wrote.
“I just reflected on how I myself had got caught up in the black and white of like, ‘This is wonderful,’” she says today. “Now having been through that trial … I’m much more neutral and agnostic.”
Scientists’ unwillingness to accept criticism makes Corlett pessimistic about the future of psychedelic research. “Science is meant to be somewhat adversarial. It’s not meant to be presided over by a single group of people,” he says. “I’m still open and excited about the possibilities, but I think this kind of breathless rush to translation and to a conclusion is really dangerous.”
And in an ethically murky turn, for those in the field who have begun to dabble in the corporate side of psychedelics, hyping up findings has become of obvious interest. Declaring conflicts of interest is standard practice in academia, and for good reason: Would you trust a paper that declared that spending more time on Instagram makes you happy if the lead author was receiving money from Meta? But that happens on a regular basis in psychedelic research; many in the field have accepted board positions or consulting fees for the ever-expanding number of psychedelic companies. That means “it’s literally a financial incentive to hype the results,” says Yaden. Watts agrees: “I think for research to be truly solid and not hyping things, it needs to be separated out from the interests of the companies who have stuff to gain.” (For complete article go to WIRED )
Expectation, Excitation, Subjectivity, Idiosyncrasy, Placebo, and the Psychedelic Micro-dosing Experiment
A systematic study of microdosing psychedelics: Taken together these findings paint an intriguing picture. We found clear changes in a small set of psychological variables: decreased depression and stress; decreased mind wandering; increased absorption; and increased neuroticism. Notably, these variables were not those that participants most expected to change. If the current findings were entirely due to expectation, then we should have seen changes in those variables that are most commonly discussed in media and online accounts of microdosing, and in those variables rated highest in Study Two. In fact several of the most commonly discussed effects of microdosing and the effects most expected to change (creativity, wellbeing, mindfulness) showed no evidence of alteration whatsoever. This suggests that the longer term changes we identified were unlikely to be due to expectation.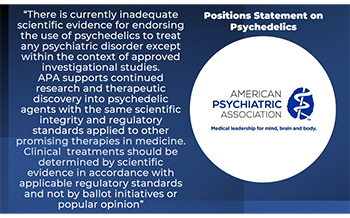
On the other hand, although we did identify clear short term changes following each microdose in the daily analyses, the longer term changes identified in Study One were unrelated to the total number of doses participants ingested during the study period and also unrelated to participants’ prior microdosing experiences. This surprising lack of a relationship between the overall quantity of microdoses and the degree of subjective effects is a reason to interpret these findings cautiously. At face value this suggests that any engagement with microdosing, whether a single dose or relatively frequent dosing, can impact the variables we identified. This may be the case, but it is also possible that participants’ self reports of dosage and frequency in this study were not precise enough to accurately characterise dose related effects.
Overall, these findings suggest several disconnects between the popular narrative around microdosing and the experience of microdosers in this sample. Participants in Study One microdosed less often than is recommended in most online protocols and did not report that many of the immediate effects of microdosing lasted beyond the day of dosing. Although popular accounts of microdosing describe sustained boosts in productivity and creativity [16–18], the longer term effects we identified mainly involved reduced mental distress and changes in constructs such as absorption and mind wandering that are not as commonly discussed. This suggests that microdosing may lead to more subtle changes characterised by improvements in mental stability, the capacity to sustain attention and increased ability to become engaged in intense imaginative experiences.
The most surprising finding was that neuroticism also appeared to increase following microdosing. This is not something that is discussed in popular accounts of microdosing and was not what participants expected in Study Two. This highlights an important and under discussed aspect of microdosing: not everyone has a positive experience. Although the majority of participants’ comments were positive (and even glowing), there were a subset of comments that reflected unease about microdosing (see Table 5). In a context of considerable hype around the practice of microdosing, particularly with regards to it’s potential as a business tool, it important to acknowledge that microdosing may not be universally beneficial. These findings highlight the need for further research into the full range of microdosing effects (positive and negative) and also for investigations into subtypes of individuals who may particularly benefit from or be adverse to the practice.
Strengths, limitations and future directions
This was very much a preliminary and exploratory study of microdosing, and there are clear limitations to the study design. This was a self reported observational study and as such, we relied on participants’ accuracy and honesty in their reports of doses and effects, and also on their continued responsiveness throughout the study period. Recruitment for this study occurred through online forums that were mainly very positive about the effects of microdosing. As such, these results may be affected by sampling bias, and may under represent individuals with negative or ambivalent experiences of microdosing. Furthermore, as might be expected in an observational study of individuals who are interested in psychedelics, there was some concurrent use of higher dose psychoactive substances and non psychedelic substances that may have had some influence on these results. A better design would certainly be to conduct an experimental study with controlled doses of known substances and a placebo comparison condition. The legal and bureaucratic limitations around psychedelic research make the approval process for such a study prohibitive. As an alternative, in implementing the current design we aimed to demonstrate that it is possible to investigate the effects of psychedelic substances in a systematic observational paradigm, using an automated and anonymous communication system.
It is clear from this research that there is a high level of popular interest in microdosing, that many people are engaged in this practice, and that there are strong expectations about the various effects that microdosing can have. The current findings suggest that popular accounts of the effects of microdosing may not match the experience of long term microdosers, and that promising avenues for future investigation are the impacts of microdosing on improved mental health, attentional capabilities, and neuroticism.
Further Reading
Psychedelics: The New Panacea – Just Like Cannabis, it will Fix Everything, Won’t it?
Download Papers
Position Use of Psychedelic Empathogenic Agents APA 2022
A Systematic Study of Microdosing 2019
E-Cigarettes labelled ‘public health crisis’...
E-Cigarettes labelled ‘public health crisis’ A damning Research has warned of the “public health crisis” E-Cigarettes are creating, putting a new generation at risk of a range of illnesses.
(Australian National University)
E-cigarettes do not improve smoking cessation, survey finds
(And worse still, Our Kids Are Getting Hooked On This Failed Harm Reduction Vehicle)
The use of e-cigarettes as a smoking cessation method did not significantly prevent relapse or successful termination, according to survey findings published in Tobacco Control.
“This is the first survey in which e-cigarettes were less popular as a smoking cessation aid than FDA-approved pharmaceutical aids,” John P. Pierce, PhD, a distinguished professor at the Herbert Wertheim School of Public Health and Human Longevity Science at UC San Diego and UC San Diego Moores Cancer Center, said in a press release. “Not only were e-cigarettes not as popular, but they were associated with less successful quitting.”

The results further showed that e-cigarettes were associated with lower abstinence rates at 12 or more months compared with pharmaceutical aids (adjusted risk difference [aRD] = 7.3%; 95% CI, 14.4 to –0.4) or any other method (aRD = 7.7%; 95% CI, 12.2 to –3.2), according to Pierce and colleagues.
Although the finding was insignificant, the researchers also noted that respondents who switched to e-cigarettes appeared to have a higher relapse rate than those who did not switch to e-cigarettes or other tobacco products. By 2019, nearly 60% of recent former smokers who used e-cigarettes daily had resumed cigarette smoking.
Also see Vaping Info Sheet
Trends in Drug Related Hospitalisations (Aust 1999-2020)
Cannabinoid Related Hospitalisations – Biggest Increase: In 2019-20, there were 6,427 cannabinoid-related hospitalisations (including cannabis and synthetic cannabinoids), which equates to an age-standardised rate of 26 hospitalisations per 100,000 people. This is the highest rate recorded over the course of monitoring and is more than double the rate observed in 1999-00 (11 hospitalisations per 100,000 people), and an increase relative to 2018-19 (24 hospitalisations per 100,000 people; p<0.001)
Major changes in Australian drug use during 2021 says annual Drug Trends reports
Significant changes include:
- The per cent reporting any use of cocaine in the past six months increased significantly from 68 per cent in 2020 to 80 per cent in 2021, the highest per cent observed since monitoring began, although frequency of use remains low.
- The per cent reporting any use of ecstasy capsules in the past six months declined significantly in 2021 (from 83 per cent in 2020 to 70 per cent in 2021), as did the per cent reporting use of ecstasy pills (53 per cent in 2020 to 42 per cent in 2021) and ecstasy powder (35 per cent in 202 to 26 per cent in 2021). The price of all forms of ecstasy significantly increased in 2021, and there were significant declines in the perceived purity and availability of ecstasy capsules and crystal, suggesting a disruption to the MDMA market compared to 2020.
- The per cent reporting use of ketamine in the past six months significantly increased from 43 per cent in 2020 to 52 per cent in 2021, representing the largest per cent reporting recent use since monitoring began. Frequency of use, however, remained low and stable at a median of three days in the past six months.
- Reported recent use of non-prescribed pharmaceutical stimulants significantly increased from 39 per cent in 2020 to 46 per cent in 2021, as did the per cent reporting any recent hallucinogenic mushroom use (30 per cent in 2020 to 45 per cent in 2021), although frequency of use remained low for both.
- Almost three-fifths (58 per cent) of the national sample reported any e-cigarette use in the six months preceding interview, a significant increase from 39 per cent in 2020. Frequency of use also increased, from a median of 7 days in 2020 to 30 days in 2021
(Dalgarno Institute Comment: It is interesting to note that even in this snapshot of the data that, from where we sit, the substances that have received ‘positive’ press, or little attention in the marketplace have increased in use. However, the substances that have had some negative focus, and restrictions placed on use ‘opportunities’, due to the pandemic (i.e. ecstasy at non-existent music festivals) have declined. Of course, interrogating the data requires more than an anecdotal swipe, but it remains an observational reality, none-the-less. Permission models continue to drive demand and extinction focused vehicles, when given even part sway, can shift demand down)
Cannabis and the Gateway Drug Theory: Correlation or Causation – Where does the Evidence Point? (DRR October 2021)
Download Report
Role of Illicit Drug Use in Domestic Violence (Aust)
Drug involvement at the most recent FDV (Family/Domestic Violence) incident was also associated with over twice the odds of injury and significantly greater negative life impact. The findings that drug use increases both the risk for and impact of FDV indicate the need for policy that advocates for interventions addressing both drug use and violence in combination.
Portugal Report
Early Onset Teen Drinking & Future Harms
Reducing Prevalence of Addiction With Youth Webinar
– Starts with ONE CHOICE
https://onechoiceprevention.org/one-choice-webinar
Exploring Psychedelic Micro-dosing & the Placebo Effect
Results of Major Study on Impact of Microdosing Published
Researchers from Imperial College London have carried out the largest placebo-controlled trial into psychedelics to date and found that small doses of LSD boost the psychology of users in a manner of ways.
However, when the researchers examined what trial volunteers took, they found placebos worked equally as well as the drug. In short, the uplift reported by microdosers might be nothing more than the placebo effect.
Balázs Szigeti, the lead author and a research associate at Imperial’s Centre for Psychedelic Research, said:
“Our findings confirmed some of the beneficial psychological effects of microdosing from anecdotal reports and observational studies, such as improved sense of wellbeing and life satisfaction.”
“But we see the same improvements among participants taking placebos. This suggests that the improvements may not be due to the pharmacological action of the drug but can instead be explained by the placebo effect.”
The trial, launched in 2018, recruited 191 members of the public who were already microdosing with LSD and able to participate online. The volunteers followed instructions to prepare gel capsules containing either a low dose of LSD, estimated at about 13μg, or a placebo. They then followed instructions to muddle up the capsules in envelopes bearing QR codes so they did not know which they took when.
During the study, the researchers used scans of the QR codes to log when each participant took a placebo versus a microdose of LSD. Throughout the four-week trial, the volunteers completed surveys on how they felt and performed a series of online cognitive tests. Typically, those on the trial reported feeling a psychological boost within a few hours of taking either LSD or placebo capsules.
The scientists found that those who microdosed for four weeks reported improved wellbeing, mindfulness and life satisfaction, along with reduced feelings of paranoia. But the placebo group also improved – to such an extent that there was no statistical difference between the two. The findings, published in eLife, suggest the expectation of taking a small dose of the drug was as good as taking the drug itself.
While the scientists believe the results are valid, they concede that the study is not as robust as a standard, laboratory-based placebo-controlled clinical study. Since the participants sourced their own drugs, it is impossible to be sure what doses each ingested, and many of the participants were evidently familiar enough with the effects of the drug to guess whether they had taken a microdose of LSD or a placebo capsule.
James Rucker, a clinician scientist who runs the psychedelic trials group at King’s College London, and was not involved in the research, said:
“This suggests that the perceived beneficial effects of microdosing psychedelics in this group are more likely to be a result of positive expectation than the capacity of the drug to induce a beneficial effect.”
While it is possible the study was too small to detect a beneficial effect, Rucker said that if that was the case, then the improvement was likely to be so small that it might not have much real world impact anyway.
“It remains to be seen whether microdosing may have therapeutic effects in patients with a defined mental health condition such as depression, or over a longer time period,” he added. “These are tractable hypotheses and we should be able to explore them with trial designs where participants receive legal microdoses of psychedelics of known purity and quality. However such studies are largely impossible under the UK government’s Schedule 1 restrictions, under which all classical psychedelics are classified.
Alcohol and Other Drug Use & Dating Violence.
- Dating violence was nearly twice as likely if either partner drank alcohol.
- Women were nearly twice as apt to perpetrate dating violence when they used drugs.
- Men were 1.4 times more likely to perpetrate dating violence when they used drugs.
- Estimated blood alcohol level and binge drinking were related to dating violence.
Introduction: Although the association between substance use and dating violence is well-established in the research literature, there is limited research establishing the temporal co-occurrence of these variables. The primary objective was to examine the temporal relationship between alcohol and drug use and subsequent dating violence using a proximal effects model.
Conclusions: These results further support an association between substance use and partner aggression at daily and situational levels of analysis, extending prior clinical findings to a college dating sample. Taken with previous research findings, our results suggest the need for college sexual assault and dating violence prevention programs to target reductions in substance use.
https://www.sciencedirect.com/science/article/pii/S2352853220301243
Hospitalizations and Deaths Associated with EVALI (Vaping/E-Cigarettes)
As of January 7, 2020, a total of 2558 hospitalized patients with nonfatal cases and 60 patients with fatal cases of e-cigarette, or vaping, product use–associated lung injury (EVALI) had been reported to the Centers for Disease Control and Prevention (CDC).
CONCLUSIONS: Chronic conditions, including cardiac and respiratory diseases and mental health conditions, were common among hospitalized patients with EVALI.
Adolescent Brain Development: WEBINAR
- Ken C. Winters (Ph.D. is a Senior Scientist at the Oregon Research Institute )
Marijuana Effects on the Endocrine and Reproductive Systems
Scientists Study How Alcohol and Cannabis Affect Adolescent Brain Responses
Executive attention and response control are critical for impulse control. Both rely on regions at the front of the brain like dorsolateral and dorsomedial frontal cortex regions. A recent Boys Town study has indicated that adolescents reporting more abuse symptoms, particularly those associated with alcohol, show problems using these brain areas during response control. Scientists note that if these regions aren't working well, an individual is less likely to control his/her impulses and may be more likely to abuse substances in the future. In addition, behavior generally becomes more impulsive.
Cannabis Genotoxicity Chromothripsis Carcinogenicity and Fetotoxicity MR FMMM
Conditional probabilities of substance use disorders and associated risk factors: Progression from first use to use disorder on alcohol, cannabis, stimulants, sedatives and opioids
- • Pre-existing mental disorders increases the risk of developing SUD.
- • Prior SUD increases the risk of transitioning from use to use disorder.
- • Highest rates of transition to SUD occurred among stimulant and opioid users.
- • Mood and anxiety disorders increased the risk of transitioning to AUD and CUD.
- • The rapidity of transition to SUD emphasizes the narrow opportunity to intervene.
Conclusion: The relative speed associated with the transition from use to SUD emphasizes the narrow window of time available to intervene, underscoring the urgency of early identification of mental health conditions and the timely provision of appropriate evidence-based interventions, which could potentially prevent the development of secondary SUDs.
The interdependence of cigarette, alcohol, and marijuana use in the context of school-based social networks
Cheng Wang1 *, John R. Hipp2,3, Carter T. Butts3,4, Cynthia M. Lakon5 1 Department of Sociology, University of Notre Dame, Notre Dame, IN, United States of America, 2 Department of Criminology, Law and Society, University of California, Irvine, Irvine, CA, United States of America, 3 Department of Sociology, University of California, Irvine, Irvine, CA, United States of America, 4 Department of Statistics, University of California, Irvine, Irvine, CA, United States of America, 5 Program in Public Health, University of California, Irvine, Irvine, CA, United States of America
Abstract: The concurrent or sequential usage of multiple substances during adolescence is a serious public health problem. Given the importance of understanding interdependence in substance use during adolescence, the purpose of this study is to examine the co-evolution of cigarette smoking, alcohol, and marijuana use within the ever-changing landscape of adolescent friendship networks, which are a primary socialization context for adolescent substance use. Utilizing Stochastic Actor-Based models, we examine how multiple simultaneous social processes co-evolve with adolescent smoking, drinking, and marijuana use within adolescent friendship networks using two school samples from early waves of the National Longitudinal Study of Adolescent to Adult Health (Add Health). We also estimate two separate models examining the effects from using one substance to the initiation and cessation of other substances for each sample.
Based on the initial model results, we simulate the model forward in time by turning off one key effect in the estimated model at a time, and observe how the distribution of use of each substance changes. We find evidence of a unilateral causal relationship from marijuana use to subsequent smoking and drinking behaviors, resulting in the initiation of drinking behavior.
Marijuana use is also associated with smoking initiation in a school with a low substance use level, and smoking cessation in a school with a high substance use level. In addition, in a simulation model excluding the effect from marijuana use to smoking and drinking behavior, the number of smokers and drinkers decreases precipitously. Overall, our findings indicate some evidence of sequential drug use, as marijuana use increased subsequent smoking and drinking behavior and indicate that an adolescent’s level of marijuana use affects the initiation and continuation of smoking and drinking
More People Are Inhaling Heroin, And It's Destroying Brain Tissue
Ed Cara Jul 10, 2018, 4:00pm
People living with opioid addiction are increasingly using the inhalation method to get high, warns a new review published Monday in JAMA Neurology. The technique known as “chasing the dragon”, which involves heating up heroin and inhaling its fumes through a pipe, may be safer in some ways than injection, but it comes with its own set of devastating side effects, including irreversible brain damage and dementia.
The doctors behind the study, led by neurologist Ciro Ramos-Estebanez of the University Hospitals Cleveland Medical Center in Ohio, were inspired to study the topic after coming across a strange case in 2015.
A young woman suffering from opioid intoxication had fallen into a coma. The coma was caused by a build up of spinal fluid in her brain, a condition known as hydrocephalus. The woman’s spinal fluid had become trapped by chronic inflammation in the brain caused by inhaling heroin.
She ultimately recovered from her coma, though with lasting cognitive impairment, after doctors performed emergency surgery that drained the lodged spinal fluid.
It was the first case of hydrocephalus linked to inhaled heroin ever reported, and it made Ramos-Estebanez and his team eager to understand the phenomenon better
Looking at more than 30 studies and case reports, which included the cases of two other patients at their hospital, the team settled on some basic observations.
For one, while there’s sparse information on how often addicts are inhaling heroin, the little data that does exist suggests it’s the fastest growing method of use, the team found.
In countries such as Sri Lanka, Norway and India, over two-thirds of heroin users admit inhaling it regularly. In the US, injection is still the most common method, but inhalation is increasing, especially in cities and areas east of the Mississippi.
It’s also becoming more popular among teens. In 2014, the team found, 21 per cent of all inpatient hospital visits due to heroin abuse among 12- to 19-year-olds involved inhalation.
The extent of damage caused by inhaling heroin also runs along a spectrum. At its mildest, it can cause memory loss and mild but long-lasting cognitive impairment; at its worst, it can kill off and create sponge-like holes in the brain’s white matter, the bundles of connective fibre that allow brain cells to talk to one another. That can lead to seizures, problems speaking, progressively worse dementia, coma and death.
Ramos-Estebanez and his team also developed a theory as how and why this damage happens. The high temperatures used to vaporise heroin, they speculate, metabolise it into a chemical that can cross the blood-brain barrier with greater ease. And because how fast it gets to the brain, these chemicals aren’t metabolised by the body into a relatively less toxic substance. The end result is a potent high that is more directly dangerous to the brain.
“Most people who take heroin intravenously don’t develop this condition,” Ramos-Estebanez said. “You’re actually washing out the dose a bit before it gets to the brain.”
Ultimately, Ramos-Estebanez wants doctors and the public to treat inhaled heroin as an emerging public health problem. Being able to recognise its signs in opioid users earlier might just be life-saving, too: Some small studies have identified a few drugs that seem capable of preventing further brain damage if administered quickly enough.
Outside of these sites, Ramos-Estebanez wants to dispel the notion that inhaling heroin is necessarily safer than other routes, such as injection. Many people, for instance, may inhale to avoid the risk of catching bloodborne diseases through contaminated needles.
“‘Chasing the dragon’ is not as safe as portrayed. And this isn’t something some doctor is saying to scare people away, it’s reality,” Ramos-Estebanez said. “It’s a heavy cost for patients, their families and society itself.”
In addition to creating accurate criteria that doctors can use to diagnose people who have brain damage caused by inhaled heroin, Ramos-Estebanez and his team are also currently trying to establish a registry so cases can be better tracked and studied.
Rates and Predictors of Conversion to Schizophrenia or Bipolar Disorder Following Substance-Induced Psychosis
Results: Overall, 32.2% (95% CI=29.7–34.9) of patients with a substance-induced psychosis converted to either bipolar or schizophrenia-spectrum disorders. The highest conversion rate was found for cannabis-induced psychosis, with 47.4% (95% CI=42.7–52.3) converting to either schizophrenia or bipolar disorder. Young age was associated with a higher risk of converting to schizophrenia. Self-harm after a substance-induced psychosis was significantly linked to a higher risk of converting to both schizophrenia and bipolar disorder. Half the cases of conversion to schizophrenia occurred within 3.1 years after a substance-induced psychosis, and half the cases of conversion to bipolar disorder occurred within 4.4 years.
Conclusions: Substance-induced psychosis is strongly associated with the development of severe mental illness, and a long follow-up period is needed to identify the majority of cases.
The Most Effective Drug Pusher Ever – Permission!
Drug Policy: Changing the Narrative
Getting enough sleep – Eating right – Little Bit of exercise, and cut down on sugar and ‘screen time’ will all help Executive Function and reduce the potential for SUD?
Adolescent Executive Dysfunction in Daily Life: Relationships to Risks, Brain Structure and Substance Use.
Abstract
During adolescence, problems reflecting cognitive, behavioural and affective dysregulation, such as inattention and emotional dyscontrol, have been observed to be associated with substance use disorder (SUD) risks and outcomes. Prior studies have typically been with small samples, and have typically not included comprehensive measurement of executive dysfunction domains. The relationships of executive dysfunction in daily life with performance based testing of cognitive skills and structural brain characteristics, thought to be the basis for executive functioning, have not been definitively determined. The aims of this study were to determine the relationships between executive dysfunction in daily life, measured by the Behaviour Rating Inventory of Executive Function (BRIEF), cognitive skills and structural brain characteristics, and SUD risks, including a global SUD risk indicator, sleep quality, and risky alcohol and cannabis use. In addition to bivariate relationships, multivariate models were tested. The subjects (n = 817; ages 12 through 21) were participants in the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study.
The results indicated that executive dysfunction was significantly related to SUD risks, poor sleep quality, risky alcohol use and cannabis use, and was not significantly related to cognitive skills or structural brain characteristics. In multivariate models, the relationship between poor sleep quality and risky substance use was mediated by executive dysfunction. While these cross-sectional relationships need to be further examined in longitudinal analyses, the results suggest that poor sleep quality and executive dysfunction may be viable preventive intervention targets to reduce adolescent substance use.
A psychological perspective on addiction – Professor Robert West
Addiction is a chronic condition, learned through experience, involving repeated powerful motivation to engage in a behaviour to an extent that causes, or risks, significant unintended harm. Addiction cannot be adequately understood in terms of any one discipline, but each of the disciplines of the behavioural and social sciences, from neuroscience to anthropology, can provide valuable insights.
For complete article and to download the PowerPoint Presentation click on the link below.
Research on Illicit Drugs
- Basic science - Bedrock of progress
- Cannabis Abusers Show Hypofrontality and Blunted Brain Responses to a Stimulant Challenge in Females but not in Males
- Chronic Methamphetamine Effects on Brain Structure and Function in Rats
- Don't Worry, Be Happy - Endocannabinoids and Cannabis at the Intersection of Stress and Reward
- Is biological ageing accelerated in drug addiction, Volkow, Klein, 2017
- Neurobiology of addiction - a neurocircuitry analysis
CANNABIS CONUNDRUM
and CANNABIS AS MEDICINE?
Check out the material on Cannabis as Medicine? at Dalgarno Institute - Cannabis as Medicine?
Check out the materian in Cannabus Conundrum at Dalgarno Institute - Cannabis Conundrum

The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services that leads public health efforts to advance the behavioral health of the nation. SAMHSA's mission is to reduce the impact of substance abuse and mental illness on America's communities.

The RiverMend Health Website - RiverMend Health is a premier provider of evidence-based, scientifically driven addiction medicine delivering world-class treatment through our nationwide network of leading addiction recovery experts and treatment centers...
Centre for Disease Control – FASDs: Information for Women
Five Things You Should Know about Drinking Alcohol during Pregnancy
- Drinking alcohol during pregnancy can cause miscarriage, stillbirth, and a range of lifelong physical, behavioral, and intellectual disabilities. These disabilities are known as fetal alcohol spectrum disorders, or FASDs. People with FASDs can have learning disabilities, hyperactivity, difficulty with attention, speech and language delays, low IQ, and poor reasoning and judgment skills. They can also have problems with their organs, including the heart and kidneys.
- There is no known safe amount of alcohol use during pregnancy or while trying to get pregnant. All drinks with alcohol can affect a baby’s growth and development and cause FASDs. A 5-ounce glass of red or white wine has the same amount of alcohol as a 12-ounce can of beer or a 1.5-ounce shot of straight liquor.
- There is no safe time to drink during pregnancy. Alcohol can cause problems for a developing baby throughout pregnancy, including before a woman knows she is pregnant. Most women will not know they are pregnant for up to 4 to 6 weeks.
- Too many women continue to drink during pregnancy. About 1 in 9 pregnant women in the United States reports alcohol use in the past 30 days. And about 1 in 26 pregnant women in the United States reports binge drinking in the past 30 days (having four or more drinks at one time).
- Fetal Alcohol Spectrum Disorders (FASDs) are completely preventable. FASDs are completely preventable if a woman does not drink alcohol during pregnancy. Why take the risk?
Esketamine for Treatment-Resistant Depression — First FDA-Approved Antidepressant in a New Class
Treating major depressive disorder remains an important challenge worldwide. The disorder impairs productivity, social functioning, and overall health, reducing life expectancy and burdening health care systems.1 Although many treatments exist, at least a third of patients do not have a response after two or more trials of antidepressant drugs and are considered to have treatment-resistant depression.2 Such patients have an increased risk of suicide relative to both the general population and patients with nonresistant major depressive disorder; at least a third of them attempt suicide.3
The FDA recently approved the S-enantiomer of ketamine, esketamine, a rapidly acting drug shown to be effective in patients with treatment-resistant depression.
Balancing these potential risks with the benefits of an effective drug for a serious disease for which there is substantial unmet need, the FDA approved esketamine with a Risk Evaluation and Mitigation Strategy (REMS). The intent of the REMS is to mitigate the risk of serious adverse outcomes resulting from sedation, dissociation, and abuse and misuse, while providing access to this effective treatment for treatment-resistant depression. Esketamine will be dispensed and administered to patients only in a medically supervised health care setting where they can be monitored for adverse reactions for at least 2 hours; pharmacies that dispense esketamine must ensure that the drug is dispensed only to clinics and hospitals that are certified in the REMS.
Published 22.5.19
Learn About E-Cigarettes!
PREVENTION ALLIANCE
Electronic cigarettes, or e-cigarettes, were invented in 2003 by Chinese inventor and pharmacist Hon Lik. Although many companies and advocates continue to bill them as a safer, smokeless alternative to traditional cigarettes, a U.S. Surgeon General report alarmingly found that 16% of high school students regularly use e-cigarettes. What’s worse, many young people who begin using nicotine through e-cigarettes will start to use traditional cigarettes later, according to the National Institute on Drug Abuse.
Smokers need help to quit, and those who can’t quit deserve a safer alternative. However, there’s a growing body of research indicating that e-cigarettes do more harm than good, and the companies selling them shamelessly advertise these products to youth in order to attract lifelong, valuable customers in ways that tobacco companies are prohibited from doing:
- E-cigarette companies use candy and fruit flavors that are known to attract youth.
- They spend millions of dollars on aggressive marketing tactics.
- They spend millions more lobbying to stop life-saving regulations.
- They produce their own research, claiming that e-cigarettes pose only a minimal risk to users despite having no long-term evidence to make that claim.
- And, their products only minimally increase the number of smokers who are able to quit.
We support the Food and Drug Administration’s crackdown on e-cigarettes because with millions of teens using e-cigarettes every year, this is the beginning of an epidemic of nicotine addiction, and we invite you to learn more about these new nicotine delivery systems from the resources below.
The US Opioid Crisis is more than it appears!
The Institute for Behavior and Health is pleased to share with you an interview of IBH President Robert L. DuPont, MD featured in Opioid Watch of The Opioid Research Institute:
The Opioid Crisis is Now About Synthetics and Polydrug Use.
Cost Legal Cannabis ILLINOIS - REPORT
Conclusion: USA – Illinois: Even under this conservative scenario, and omitting important cost centers such as long-term health costs, marijuana legalization will cost Illinois approximately $670.5 million in 2020, significantly more than the $566 million in revenues that pro-legalization activists project.
The Moral Hazard of Lifesaving Innovations: Naloxone Access, Opioid Abuse, and Crime
March 6, 2018 - Abstract
Naloxone access may unintentionally increase opioid abuse through two channels: (1) saving the lives of active drug users, who survive to continue abusing opioids, and (2) reducing the risk of death per use, thereby making riskier opioid use more appealing. By increasing the number of opioid abusers who need to fund their drug purchases, Naloxone access laws may also increase theft. We exploit the staggered timing of Naloxone access laws to estimate the total effects of these laws. We find that broadening Naloxone access led to more opioid-related emergency room visits and more opioid-related theft, with no reduction in opioid-related mortality.
Nutrition in Addiction Recovery
This document has been prepared to educate people about how drugs and alcohol can disrupt the normal functioning of the body and how better nutrition can help diminish some of these biochemical and digestive problems. This document only focuses on one specific component of a comprehensive recovery treatment program—better nutrition. It is not intended to be used as a substitute for a doctor’s advice or as a recovery treatment program.
Beyond Supply: How We Must Tackle the Opioid Epidemic
A. Benjamin Srivastava, MDCorrespondence information about the author MD A. Benjamin Srivastava
Email the author MD A. Benjamin Srivastava, Mark S. Gold, MD
Department of Psychiatry, Washington University School of Medicine, St Louis, MO
DOI: https://doi.org/10.1016/j.mayocp.2018.01.018
The opioid epidemic is the most important and most serious public health crisis today. The effects are reported in overdose deaths but are also starkly evident in declines in sense of well-being and general health coupled with increasing all-cause mortality, particularly among the middle-aged white population.1 As exceptionally well described by Rummans et al in this issue of Mayo Clinic Proceedings, the cause of the epidemic is multifactorial, including an overinterpretation of a now infamous New England Journal of Medicine letter describing addiction as a rare occurrence in hospitalized patients treated with opioids, initiatives from the Joint Commission directed toward patient satisfaction and the labeling of pain as the “5th vital sign,” the advent of extended-release oxycodone (OxyContin), an aggressive marketing campaign from Purdue Pharma L.P., and the influx of heroin and fentanyl derivatives.
To date, most initiatives directed toward fighting the opioid initiatives, and the focus of the discussion from Rummans et al, have targeted the “supply side” of the equation. These measures include restricting prescriptions, physician drug monitoring programs, and other regulatory actions. Indeed, although opioid prescriptions have decreased from peak levels, the prevalence of opioid misuse and use disorder remains extremely prevalent (nearly 5%). Further, fatal drug overdoses, to which opioids contribute to a considerable degree, continue to increase, with 63,000 in 2016 alone.6 Thus, although prescription supply and access are necessary and important, we need to address the problem as a whole. To this point, for example, the ease of importation and synthesis of very cheap and powerful alternatives (eg, fentanyl and heroin) and the lucrative US marketplace have contributed to the replacement pharmacy sales and diversion with widespread street-level distribution of these illicit opioids; opioid-addicted people readily switch to these illicit opioids.
A complementary and necessary approach is to target the “demand” side of opioid use, namely, implementation of preventive measures, educating physicians, requiring physician continuing education for opioid prescribing licensure, and addressing why patients use opioids in the first place. Indeed, prevention of initiation of use is the only 100% safeguard against addiction; however, millions of patients remain addicted, and they need comprehensive, rather than perfunctory, treatment. Rummans and colleagues are absolutely correct in their delineation of the unwitting consequences of a focus on pain, given that a perceived undertreatment of pain fueled the opioid epidemic in the first place. They are correct to point out how effective pain evaluation and treatment are much more than prescribing and should routinely include psychotherapy, interventional procedures, and nonopioid therapies. In addition, we have described the crossroads between pain and addiction as well as successful strategies to manage patients with both chronic pain syndromes and addiction.
The Key Role of Prevention In Addressing the Current Landscape of Substance Abuse in America: A Perspective
Presented 2018 Annual PREVENTION DAY February 2018
Elinore F. McCance-Katz, MD, PhD – Assistant Secretary for Mental Health and Substance Use
Substance Abuse and Mental Health Services Administration (U.S. Department of Health and Human Services)
Reducing Addiction Must Begin with Youth Prevention
Iceland knows how to stop teen substance abuse but the rest of the world isn’t listening!
Today, Iceland tops the European table for the cleanest-living teens. The percentage of 15- and 16-year-olds who had been drunk in the previous month plummeted from 42 per cent in 1998 to 5 per cent in 2016. The percentage who have ever used cannabis is down from 17 per cent to 7 per cent. Those smoking cigarettes every day fell from 23 per cent to just 3 per cent.
The way the country has achieved this turnaround has been both radical and evidence-based, but it has relied a lot on what might be termed enforced common sense. “This is the most remarkably intense and profound study of stress in the lives of teenagers that I have ever seen,” says Milkman. “I’m just so impressed by how well it is working.”
If it was adopted in other countries, Milkman argues, the Icelandic model could benefit the general psychological and physical wellbeing of millions of kids, not to mention the coffers of healthcare agencies and broader society. It’s a big if.



